4 minutes read time
Central nervous system (CNS) depressants are commonly prescribed medications for elderly patients to manage conditions such as anxiety, insomnia, chronic pain, and behavioural disturbances. While beneficial individually, these medications – when combined – can lead to CNS-active polypharmacy, significantly raising the risk of serious adverse outcomes in elderly patients.
MIMS Clinical Decision Solutions (CDS) empowers prescribers across Southeast Asia to deliver safer care, especially for elderly patients vulnerable to medication risks. Through tools like the Drug Duplicate Alert Module and Drug Interaction Alert Module, MIMS CDS enables clinicians to detect, manage, and reduce these risks directly at the point of prescribing.
What are CNS Depressants?
CNS depressants include medications such as benzodiazepines, opioids, hypnotics, antidepressants, and antipsychotics. They slow brain activity, producing effects ranging from sedation and anxiety relief to pain management and sleep improvement.
What is CNS-active Polypharmacy?
CNS-active polypharmacy is defined as the concurrent use of three or more CNS-active medications over an extended period, typically exceeding 30 consecutive days. Elderly patients are particularly vulnerable due to age-related physiological changes affecting drug metabolism and sensitivity, making adverse effects more severe [1][2].
Common CNS Medications Prescribed to Older Adults
Clinicians commonly prescribe the following CNS-active medications to elderly patients:
- Benzodiazepines: Diazepam, Alprazolam, Lorazepam
- Opioids: Morphine, Oxycodone, Tramadol
- Hypnotics: Zolpidem, Zopiclone
- Antidepressants: Sertraline, Amitriptyline, Mirtazapine
- Antipsychotics: Risperidone, Olanzapine, Quetiapine
Prevalence of CNS-active Polypharmacy
The prevalence of CNS-active polypharmacy remains notably high among elderly patients. In particular, a study in the United States showed that between 21.2% and 25.0% of individuals with early-onset dementia were prescribed multiple CNS-active medications, and these rates remained relatively stable from 2013 to 2020 [1].
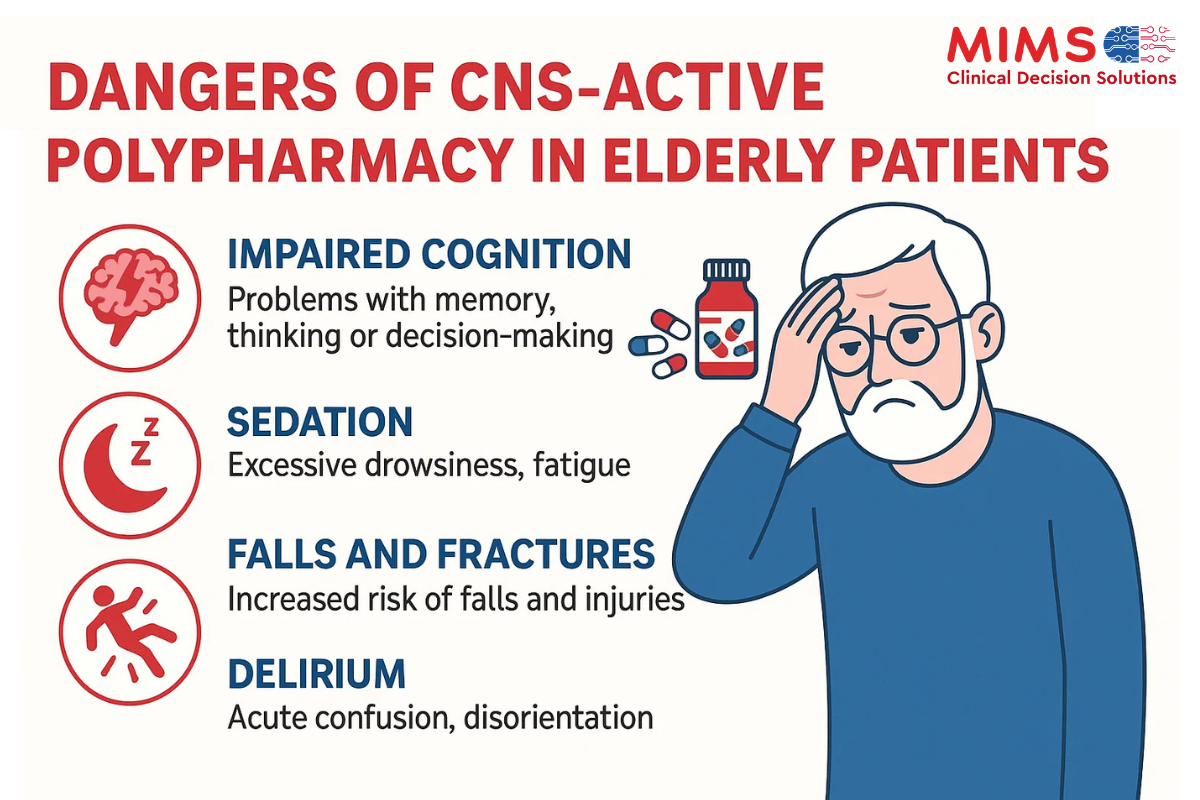
Dangers of CNS-active Polypharmacy in Elderly Patients
Elderly patients exposed to CNS-active polypharmacy face significant risks:
- Cumulative Sedation Risk: Combining multiple CNS depressants can cause excessive sedation, impairing cognitive and physical functioning [2].
- Increased Risk of Falls and Fractures: Sedation and balance impairment dramatically increase the risk of falls and subsequent fractures, which are associated with substantial morbidity and mortality among older adults [3].
- Cognitive Impairment and Confusion: Chronic polypharmacy can exacerbate cognitive dysfunction, confusion, and memory impairment, significantly reducing quality of life [2].
- Respiratory Depression: The concurrent use of opioids and benzodiazepines significantly elevates the risk of severe respiratory depression, which can be fatal [4].
Strategies to Minimise CNS-active Polypharmacy
Clinicians can reduce the risks associated with CNS-active polypharmacy through several evidence-based strategies:
- Regular Medication Reviews: Periodic assessments to identify inappropriate or duplicate CNS medications, facilitating safer prescribing practices [3].
- Deprescribing: Planned reduction or cessation of medications that are no longer necessary or that pose greater risks than benefits [3].
- Careful Medication Selection: Choosing medications with lower adverse effect profiles and considering non-pharmacological alternatives when appropriate [3].
- Patient Education: Educating patients and caregivers on medication risks, promoting adherence, and fostering informed decision-making [3].
Leveraging Clinical Decision Solutions (CDS)
MIMS Clinical Decision Solutions (CDS) provides prescribers with robust tools specifically designed to mitigate CNS-active polypharmacy risks:
- Drug Interaction Alert Module: Highlights clinically significant interactions between CNS depressants, providing actionable recommendations to manage or avoid adverse drug interactions effectively.
- Drug Duplicate Alert Module: Proactively identifies when multiple CNS depressants within the same pharmacological class are prescribed concurrently, reducing unnecessary medication duplication.
Utilising both modules together ensures safer prescribing practices, which is particularly critical for elderly patients with complex medication regimens.
Conclusion
CNS-active polypharmacy poses serious risks to elderly patients, increasing the likelihood of sedation, cognitive impairment, falls, and respiratory depression.
By integrating regular medication reviews, deprescribing practices, careful medication selection, patient education, and leveraging advanced CDS tools such as MIMS CDS‘s Drug Duplicate Alert Module and Drug Interaction Alert Module, healthcare providers can significantly improve medication safety and patient outcomes.
References
- Wei YJ, Shrestha N, Chiang C, et al. Prevalence and trend of central nervous system-active medication polypharmacy among US commercially insured adults with vs without early-onset dementia: a multi-year cross-sectional study. Alzheimers Res Ther. 2024 Feb 8;16(1):30. See more.
- Wright RM, Roumani YF, Boudreau R, Newman AB, Ruby CM, Studenski SA, Shorr RI, Bauer DC, Simonsick EM, Hilmer SN, Hanlon JT; Health, Aging and Body Composition Study. Effect of central nervous system medication use on decline in cognition in community-dwelling older adults: findings from the Health, Aging And Body Composition Study. J Am Geriatr Soc. 2009 Feb;57(2):243-50. See more.
- Jandu JS, Mohanaselvan A, Dahal R, et al. Strategies to Reduce Polypharmacy in Older Adults. [Updated 2024 Aug 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan. See more.
- Gudin JA, Mogali S, Jones JD, et al. Risks, management, and monitoring of combination opioid, benzodiazepines, and/or alcohol use. Postgrad Med. 2013 Jul;125(4):115-30. See more.
